HOVON HO121 CLL
Main info
- Identifier:
- HO121 CLLM1
- Sponsor:
- HOVON
- Working group party:
- CLL
- Age:
- >= 18
- Stage:
- 2nd Line
- Echelon:
- Limited Site Selection
- Included patients:
-
89(of 200)
- Active sites:
-
22(of 21)
- Title:
A phase 3, multicenter, randomized, double-blind, placebo-controlled, parallel-group study of the efficacy and safety of lenalidomide (Revlimid®) as maintenance therapy for high-risk patients with chronic lymphocytic leukemia following first-line therapy.
Timeline
News
The HO121 study is closed
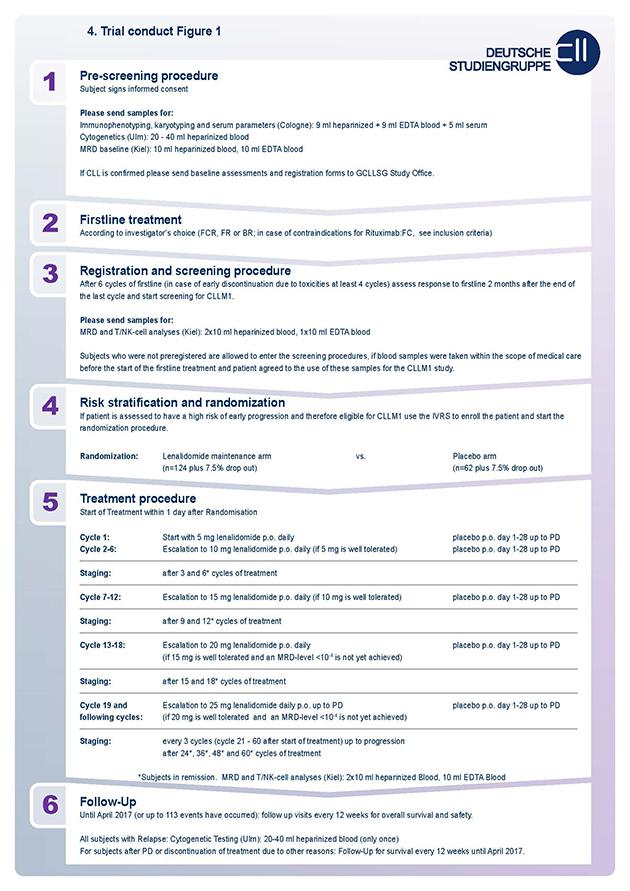
Flow
Details
- Phase:
- Prospective Phase III study
- Monitoring Type:
- Study Specific
- Objectives:
Primary objective
- To compare the efficacy of lenalidomide versus placebo maintenance therapy.
The primary efficacy objective of this study is to investigate if lenalidomide maintenance therapy is supersior to placebo maintenance therapy in prolonging PFS, for subjects with a high risk of early progression following first-line treatment. All subjects, including both subjects who do and do not achieve MRD negativity will be treated up to disease progression with maintenance.
Secondary objective
- To evaluate the prolongation of overall survival (OS) of lenalidomide versus placebo maintenance therapy.
- To evaluate the safety of lenalidomide versus placebo maintenance therapy.
Eligibility
- Inclusion Criteria:
- Must understand and voluntarily sign an informed consent form.
- Age ≥ 18 years at the time of signing the informed consent form.
- Must be able to adhere to the study visit schedule and other protocol requirements.
- Must have a documented diagnosis of CLL (IWCLL guidelines for the diagnosis and treatment of chronic lymphocytic leukemia1.
- Must have been treated with one of the first line induction therapies: fludarabine/cyclophosphamide, fludarabine/rituximab, fludarabine/cyclophosphamide/rituximab, pentostatin/cyclophosphamide/rituximab or bendamustine/rituximab.
- Must have achieved a response of at least PR ((IWCLL guidelines for the diagnosis and treatment of chronic lymphocytic leukemia) following completion (minimum 4 cycles) of first line induction therapy prior to randomization, and have either:
- MRD levels in the peripheral blood at final restaging of ≥10-2 or
- MRD levels in the peripheral blood at final restaging of ≥10-4 - <10-2 combined with an unmutated IGHV-status or 17p-deletion or TP53 mutation.
- Must have completed last cycle of at least 4 cycles of first-line induction no less than 8 weeks (56 days) and no greater than 20 weeks (140 days) prior to randomization.
- Subjects who completed first-line induction treatment with less than 6 cycles but at least 4 cycles should document reason for early discontinuation.
- Must have an Eastern Cooperative Oncology Group (ECOG see appendix 11.13) performance status score of ≤2.
- Negative serological Hepatitis B test or negative PCR in case of positive serological test without evidence of an active infection, negative testing of Hepatitis C RNA, negative HIV test within 6 weeks prior to randomization.
- Females of childbearing potential (FCBP)† must:
- Have two negative medically supervised pregnancy tests prior to starting of study therapy. She must agree to ongoing pregnancy testing during the course of the study, and after end of study therapy. This applies even if the subject practices complete and continued sexual abstinence.
- Either commit to continued abstinence from heterosexual intercourse (which must be reviewed on a monthly basis) or agree to use, and be able to comply with, two reliable forms of effective contraception simultaneously to achieve a PEARL-Index <1 without without interruption (Highly effective methods: Intrauterine device (IUD), Hormonal (birth control pills, injections, implants), Tubal ligation, Partner’s vasectomy, Additional effective methods: Male condom, Diaphragm, Cervical Cap). 28 days prior to starting study drug, during the study therapy (including dose interruptions), and for 28 days after discontinuation of study therapy.
- Male subjects must:
- Agree to use a condom during sexual contact with a FCBP, even if they have had a vasectomy, throughout study drug therapy, during any dose interruption and after cessation of study therapy.
- Agree to not donate semen during study drug therapy and for a period after end of study drug therapy.
- All subjects must:
- Have an understanding that the study drug could have a potential teratogenic risk.
- Agree to abstain from donating blood while taking study drug therapy and following discontinuation of study drug therapy.
- Agree not to share study medication with another person.
- Be counseled about pregnancy precautions and risks of fetal exposure.
- Willingness to inform the general practicioner
†Definition: This protocol defines a female of childbearing potential as a sexually mature woman who: 1) has not undergone a hysterectomy or bilateral oophorectomy or 2) has not been naturally postmenopausal (amenorrhea following cancer therapy does not rule out childbearing potential) for at least 24 consecutive months (i.e., has had menses at any time in the preceding 24 consecutive months).
- Exclusion Criteria:
- A CIRS Score of more than 6 or a single score of 4 for an organ system limiting the ability to receive an intensive treatment
- Active infections requiring systemic antibiotics.
- Systemic infection CTC grade 3 or 4 that has not resolved > 2 months prior to randomization in spite of adequate anti-infective therapy.
- Autologous or allogeneic bone marrow transplant as first line therapy.
- Pregnant or lactating females.
- Systemic treatment for CLL in the interval between completing the last cycle of first-line induction therapy and randomization.
- Participation in any clinical study or having taken any investigational therapy which would interfere with the study drug for a disease other than CLL within 28 days prior to initiating maintenance therapy.
- Known presence of alcohol and/or drug abuse.
- Central nervous system (CNS) involvement as documented by spinal fluid cytology or imaging. Subjects who have signs or symptoms suggestive of leukemic meningitis or a history of leukemic meningitis must have a lumbar puncture procedure performed within two weeks prior to randomization.
- Prior history of malignancies, other than CLL, unless the subject has been free of the disease for ≥5 years. Exceptions include the following:
- Basal cell carcinoma of the skin
- Squamous cell carcinoma of the skin
- Carcinoma in situ of the cervix
- Carcinoma in situ of the breast
- Incidental histological finding of prostate cancer (TNM stage of T1a or T1b)
- History of renal failure requiring dialysis.
- Prior therapy with lenalidomide.
- Any of the following laboratory abnormalities:
- Calculated (method of Cockroft-Gault) creatinine clearance of <60 mL/min
- Absolute neutrophil count (ANC) < 1,000/μL (1.0 X 10^9/L)
- Platelet count < 50,000/μL (50 X 10^9/L)
- Serum aspartate aminotransferase (AST)/serum glutamic-oxaloacetic transaminase (SGOT) or alanine transaminase (ALT)/serum glutamate pyruvate transaminase (SGPT) > 3.0 x upper limit of normal (ULN)
- Serum total bilirubin > 2.0 mg/dL (with the exception of Gilbert’s Syndrome)
- Uncontrolled hyperthyroidism or hypothyroidism.
- Venous thromboembolism within one year.
- ≥ Grade-2 neuropathy.
- Uncontrolled autoimmune hemolytic anemia or thrombocytopenia.
- Disease transformation (active) (i.e. Richter’s Syndrome, prolymphocytic leukemia).
- Known allergy to allopurinol if the subject has bulky disease.
- Prisoners, or subjects who are institutionalized by regulatory or court order or persons who are who are in dependence to the sponsor or an investigator.
Registration Details
The registration form and the screening pages 1-16 (marked with “PRE” and “SCREENING” of the CRFs) should be faxed to the GCLLSG Central Study Office.
Participating Sites
Ziekenhuizen die deelnemen aan het onderzoek staan benoemd op de HOVON website bij het onderzoek. Het kan zijn dat uw ziekenhuis niet genoemd wordt, maar wel aan het onderzoek deelneemt. Informeer hiernaar bij uw arts.
